In Figure 1, influenza viruses bind to specific carbohydrate structures on the surface of airway cells to gain entry. In Figure 2, nanotrap particles effectively mimic the cell surface so that their carbohydrate structures "trap" viruses and prevent infection.Newly emerging flu viruses could soon be countered by a treatment that Charles Stark Draper Laboratory is developing that “traps” viruses before they can infect host cells.
Further into the future, patients suffering from any type of virus could be cured with DRACO, a drug also under development at Draper that is designed to rapidly recognize and eliminate cells infected by virtually any virus.
Both methods could help safeguard against bioterrorist attacks and naturally occurring pandemics in a manner that is unlikely to lead to treatment-resistant strains. Initial testing on the treatments, which each use tiny, non-toxic particles that can be injected, inhaled, or eaten, has shown them to be effective and safe against a multitude of strains of disease.
Nanotraps, which could be taken at the first sign of infection or exposure, is likely the first of the products ready for use, and is expected to begin clinical trials in two to five years (from 01/07/2014) , according to Jim Comolli, who leads the research on the effort at Draper.
Nanotraps, developed by a team of researchers from Draper, Massachusetts Institute of Technology, the Univ. of Massachusetts Medical School, and the Univ. of Santa Barbara, are nanoparticles that act as viral “traps” using specific molecules found naturally within the human body. A paper published in the March issue of Journal of Biological Chemistry (First Published on January 28, 2013 doi: 10.1074/jbc.M112.437202) detailed their findings.
The nanotraps look like the surface of a cell, with numerous carbohydrate molecules attached that closely resemble those targeted by flu viruses in the human respiratory system. These molecules, initially characterized in the Sasisekharan Lab at MIT, act as bait for the flu virus, which bind to the nanotrap instead of a host cell and are cleared away with mucus, preventing infection, Comolli said.
The research team has demonstrated in the laboratory that the nanotraps effectively countered multiple influenza strains able to infect humans and went on to show nanotraps protected mice infected with the flu. They have also developed additional particles geared toward other types of respiratory viruses.
Nanotraps, unlike most vaccines, are not strain specific and are designed to be effective against newly emerging strains of human-adapted influenza virus. Since nanotraps mimic a fundamental step in the viral life cycle—the binding of the virus to a host cell’s receptor—nanotraps may offer an opportunity to treat devastating infectious diseases without causing the development of treatment resistance, Comolli said.
The nanotrap molecule is composed mainly of compounds found naturally in the human body so it is likely to be safe as an inhalant, topical solution, or intravenous treatment and inexpensive to manufacture. With further development, nanotraps have the potential to treat a large range of infectious diseases because the attached carbohydrates can be tuned for other viruses such as HIV, Respiratory Syncytial Virus (RSV), and Herpes Simplex Virus (HSV), as well as bacteria and toxins.
The work was originally funded by the Defense Advanced Research Projects Agency (DARPA) to address emerging pandemics or bioweapons targeting US troops; Draper is continuing the research with the intent of applying it more broadly to the civilian community.
While nanotraps could be customized to treat a variety of viruses, another project underway at Draper, DRACO could do so with a single approach. DRACO is a unique therapeutic drug that should be effective against a very broad spectrum of viruses, just as existing antibiotics are effective against a broad range of bacterial infections. DRACO could be ready for human clinical trials in five to 10 years, according to Todd Rider, who leads the research at Draper.
DRACO (Double-stranded RNA Activated Caspase Oligomerizer) is designed to detect cells that have been virally infected and then eradicate only the infected cells, rapidly ending the infection. DRACO has proven effective in vivo against influenza and three hemorrhagic fever viruses, and in vitro against 15 different viruses—including common cold viruses, the H1N1 influenza strain, adenoviruses, a mouse polio virus, dengue fever, and stomach viruses, among others. It has also been tested and proven safe in both mice and 11 different human and animal cell types representing organs like the heart, lungs, liver, and kidney, among others.
DRACO is designed to be attracted to a specific type of RNA exclusive to viral infections—long double-stranded RNA, or dsRNA. Detecting this dsRNA in a human or animal cell indicates that that host cell has been taken over by a virus and is now in the process of creating more viruses. DRACO enters cells and attaches itself to any dsRNA. Once two or more DRACOs attach to the dsRNA, they interact with one another and activate a natural self-destruct switch inside the infected cell, terminating the infected cell and the virus that it was helping to reproduce.
DRACO is designed to be both broad-spectrum and nontoxic to humans—overcoming existing issues with current anti-viral treatments. Because DRACO is so broad-spectrum and acts so rapidly, there is little opportunity for the virus to evolve defenses against this treatment, Rider said.
Rider is expanding his DRACO research and testing more strains of various viruses in cells and animals.
DRACO has been funded by grant AI057159 from the National Institute of Allergy and Infectious Diseases and the New England Regional Center of Excellence for Biodefense and Emerging Infectious Diseases, with other funding coming from DARPA, the Defense Threat Reduction Agency, and the office of the Director of Defense Research and Engineering.
Source: Charles Stark Draper Laboratory
Further into the future, patients suffering from any type of virus could be cured with DRACO, a drug also under development at Draper that is designed to rapidly recognize and eliminate cells infected by virtually any virus.
Both methods could help safeguard against bioterrorist attacks and naturally occurring pandemics in a manner that is unlikely to lead to treatment-resistant strains. Initial testing on the treatments, which each use tiny, non-toxic particles that can be injected, inhaled, or eaten, has shown them to be effective and safe against a multitude of strains of disease.
Nanotraps, which could be taken at the first sign of infection or exposure, is likely the first of the products ready for use, and is expected to begin clinical trials in two to five years (from 01/07/2014) , according to Jim Comolli, who leads the research on the effort at Draper.
Nanotraps, developed by a team of researchers from Draper, Massachusetts Institute of Technology, the Univ. of Massachusetts Medical School, and the Univ. of Santa Barbara, are nanoparticles that act as viral “traps” using specific molecules found naturally within the human body. A paper published in the March issue of Journal of Biological Chemistry (First Published on January 28, 2013 doi: 10.1074/jbc.M112.437202) detailed their findings.
The nanotraps look like the surface of a cell, with numerous carbohydrate molecules attached that closely resemble those targeted by flu viruses in the human respiratory system. These molecules, initially characterized in the Sasisekharan Lab at MIT, act as bait for the flu virus, which bind to the nanotrap instead of a host cell and are cleared away with mucus, preventing infection, Comolli said.
The research team has demonstrated in the laboratory that the nanotraps effectively countered multiple influenza strains able to infect humans and went on to show nanotraps protected mice infected with the flu. They have also developed additional particles geared toward other types of respiratory viruses.
Nanotraps, unlike most vaccines, are not strain specific and are designed to be effective against newly emerging strains of human-adapted influenza virus. Since nanotraps mimic a fundamental step in the viral life cycle—the binding of the virus to a host cell’s receptor—nanotraps may offer an opportunity to treat devastating infectious diseases without causing the development of treatment resistance, Comolli said.
The nanotrap molecule is composed mainly of compounds found naturally in the human body so it is likely to be safe as an inhalant, topical solution, or intravenous treatment and inexpensive to manufacture. With further development, nanotraps have the potential to treat a large range of infectious diseases because the attached carbohydrates can be tuned for other viruses such as HIV, Respiratory Syncytial Virus (RSV), and Herpes Simplex Virus (HSV), as well as bacteria and toxins.
The work was originally funded by the Defense Advanced Research Projects Agency (DARPA) to address emerging pandemics or bioweapons targeting US troops; Draper is continuing the research with the intent of applying it more broadly to the civilian community.
While nanotraps could be customized to treat a variety of viruses, another project underway at Draper, DRACO could do so with a single approach. DRACO is a unique therapeutic drug that should be effective against a very broad spectrum of viruses, just as existing antibiotics are effective against a broad range of bacterial infections. DRACO could be ready for human clinical trials in five to 10 years, according to Todd Rider, who leads the research at Draper.
DRACO (Double-stranded RNA Activated Caspase Oligomerizer) is designed to detect cells that have been virally infected and then eradicate only the infected cells, rapidly ending the infection. DRACO has proven effective in vivo against influenza and three hemorrhagic fever viruses, and in vitro against 15 different viruses—including common cold viruses, the H1N1 influenza strain, adenoviruses, a mouse polio virus, dengue fever, and stomach viruses, among others. It has also been tested and proven safe in both mice and 11 different human and animal cell types representing organs like the heart, lungs, liver, and kidney, among others.
DRACO is designed to be attracted to a specific type of RNA exclusive to viral infections—long double-stranded RNA, or dsRNA. Detecting this dsRNA in a human or animal cell indicates that that host cell has been taken over by a virus and is now in the process of creating more viruses. DRACO enters cells and attaches itself to any dsRNA. Once two or more DRACOs attach to the dsRNA, they interact with one another and activate a natural self-destruct switch inside the infected cell, terminating the infected cell and the virus that it was helping to reproduce.
DRACO is designed to be both broad-spectrum and nontoxic to humans—overcoming existing issues with current anti-viral treatments. Because DRACO is so broad-spectrum and acts so rapidly, there is little opportunity for the virus to evolve defenses against this treatment, Rider said.
Rider is expanding his DRACO research and testing more strains of various viruses in cells and animals.
DRACO has been funded by grant AI057159 from the National Institute of Allergy and Infectious Diseases and the New England Regional Center of Excellence for Biodefense and Emerging Infectious Diseases, with other funding coming from DARPA, the Defense Threat Reduction Agency, and the office of the Director of Defense Research and Engineering.
Source: Charles Stark Draper Laboratory
| United States Patent | 9,408,890 |
| Comolli , et al. | August 9, 2016 |
Multivalent liposome formulations
| Inventors: | Comolli; James (Boxborough, MA), Trevejo; Jose (Brighton, MA), Sasisekharan; Ram (Cambridge, MA), Shriver; Zachary (Winchester, MA), Viswanathan; Karthik(Waltham, MA), Fygenson; Deborah (Santa Barbara, CA), Finberg; Robert (Newtonville, MA), Wang; Jennifer (Shrewsbury, MA) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Applicant: |
| ||||||||||
| Assignee: | The Charles Stark Draper Laboratory, Inc. (Cambridge, MA) The Massachusetts Institute of Technology (Cambridge, MA) University of California, Santa Barbara (UCSB) (Santa Barbara, CA) University of Massachusetts Medical School (Boston, MA) | ||||||||||
| Family ID: | 50097850 | ||||||||||
| Appl. No.: | 14/161,555 | ||||||||||
| Filed: | January 22, 2014 |
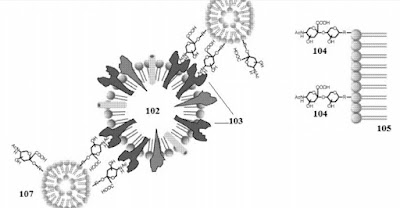
The multivalent liposome composition of the present technology has enhanced binding due to the multivalent display of binding targets and the mobility of the binding targets on the surface of the liposome. Multivalency is the display of at least two binding targets on the surface of the liposome. By way of example, but not by way of limitation, FIGS. 1A-C illustrate the enhanced inhibitory effect of multivalent liposome compositions. Referring to FIG. 1A, influenza virus 102 infects host cells by first attaching to .alpha.2-6 terminally linked SA 104 on the cell membrane 105 through HA 103. Liposomes 101 that do not contain LSTc, in general, have low effect in inhibiting influenza virus adhesion or infection.
With reference to FIG. 1B, monovalent LSTc liposomes 106 bind to the HA receptors 103 of the influenza virus 102.
With reference to FIG. 1C, a single multivalent LSTc liposome composition 107, e.g., with 5 mol % or more LSTc on the surface, are capable of competitively binding multiple HA receptors 203 of the influenza virus 102. The presence of multiple binding targets on the surface of a single liposome allows a single liposome to have enhanced, efficient, and high affinity binding to the virus, bacteria, or toxin as compared to the monovalent LSTc liposome of FIG. 1B.
C.
What is claimed is:
1. A composition comprising: a first population of lipids, a second population of lipids, cholesterol, and two or more influenza A binding targets, wherein the influenza A binding targets are linked to the first population of lipids to form BT-lipids, wherein the BT-lipids, the second population of lipids, and cholesterols form a liposome, wherein the binding targets are displayed on the outer surface of the liposome, wherein the first population of lipids and the second population of lipids in the liposome have a phase transition temperature below 41.degree. C., wherein the cholesterol comprises 15 to 30 mol % of the liposome.
Patent Family:



No comments:
Post a Comment